Scar after a surgery
All about the scar
What is a scar ?
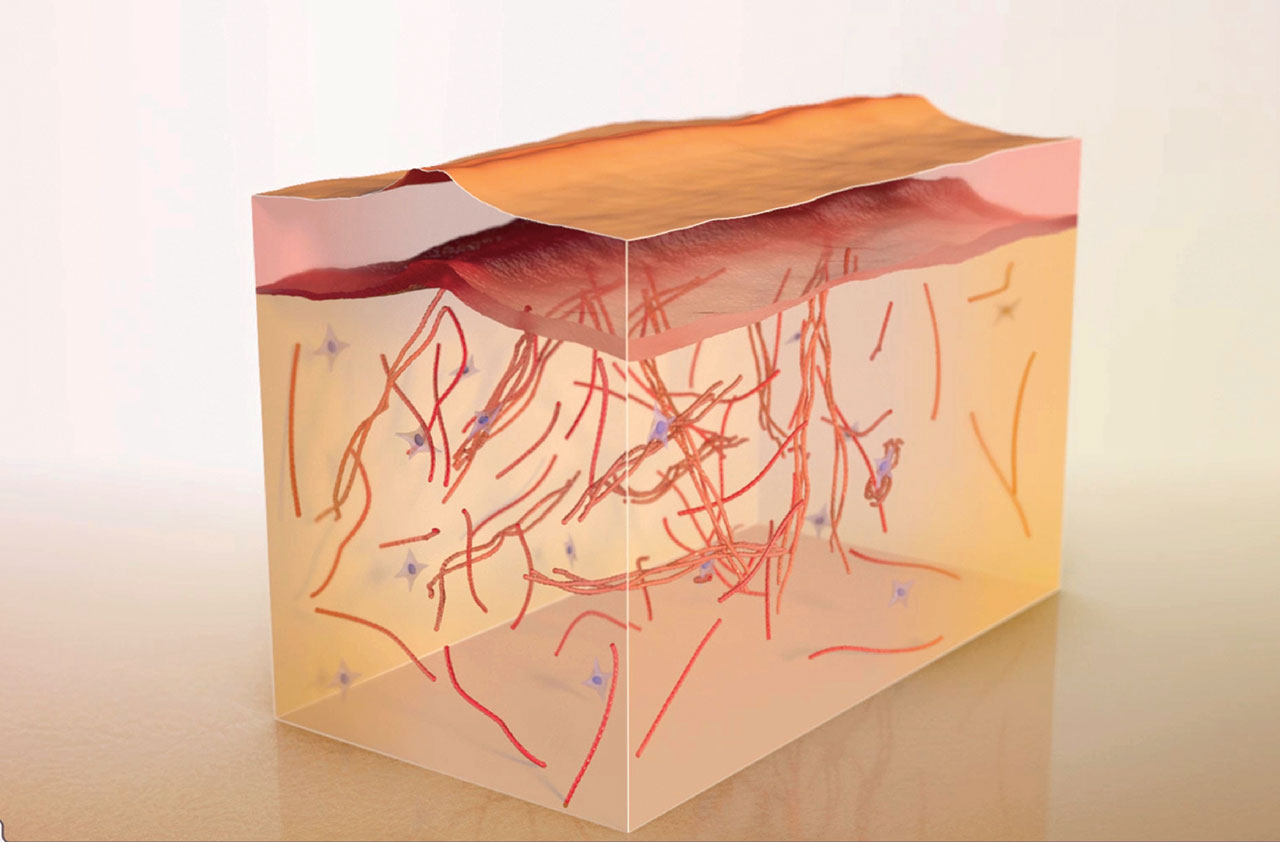
In order to quickly close the wound after an incision, the skin cells multiply and synthesize the elements that surround them, such as collagen or elastin. A new fibrous tissue is created: the scar. Any surgical incision will lead to the formation of a scar, the final appearance of which will depend on several factors :
- its anatomical location (zones of tension, skin folds etc.)
- operative gesture (technique, suture, staples)
- post-operative treatments
- intrinsic factors related to the patient (age, genetic predispositions, phototype, ethnicity, hormonal treatment, medical history etc.). It is on these factors (your skin, your way of healing) that UrgoTouch ® will act !
- extrinsic factors such as environmental factors (e.g. sun exposure) and behavioral factors (e.g. tobacco).
What is the healing process like ?
The scar healing process for a surgical wound goes through 3 main phases.
The first phase begins immediately after surgery and lasts around 2 weeks. The skin cells multiply and synthesize the main components of the dermis (collagen and elastin fibers in particular). The scar is generally neat and slightly visible.
Then, over the first few months following the surgery, the scar changes, a sign of deep-down remodeling. The scar becomes inflammatory, which means redder, sometimes harder, more raised and is often itchy. The scar will be slightly higher than the surrounding skin. During the scar healing process, the color of the scar will fade and its volume will decrease. This stage lasts for an average of 3 to 6 months.
The scar then enters its final phase when it begins to become paler and softer (remodeling). At the end of this process, which varies in duration and can take up to 2 years, the scar will take on its final appearance: paler, softer and insensitive.

And what about UrgoTouch ® ?
It is at the very beginning of the first and inflammatory phase that UrgoTouch ® will act on. Its goal is to improve the organization of collagen fibers, by biomodulating the scar, at the earliest stage of healing, just after the suture.
What is an ideal scar ?
In a perfect world, scars would not exist. But here is what a mature surgical scar should look like from a cosmetic point of view:
- a parallel disposition to the folds and lines of tension of a relaxed skin
- an unnoticeable fine line
- an elevation similar to the surrounding skin
- a color similar to that of the surrounding skin : no hypo/hyper pigmentation
In summary, an ideal is a scar that matches as much as possible with the surrounding skin!

Problematic scars: pathological scars
In some cases, the scar evolves abnormally and can become ugly.
The history of existing scars can be a predictive indicator of future scars. That’s why your surgeon will always pay special attention to it.
But beware, the absence of previous pathological scars does not exclude the risk of future pathological scars, because the risk factors may have changed: for example a new incision on a zone of high tension, aging, increased tobacco intake, medicines etc.
What are these complications?
There are in particular three cases of complications, more or less frequent and severe.
Linear hypertrophic scars
How does it look like ?
The scar takes the appearance of an overly thick cord, of increased and variable width.
When does it come to light ?
They are usually detected in the weeks (or months) following the surgery.
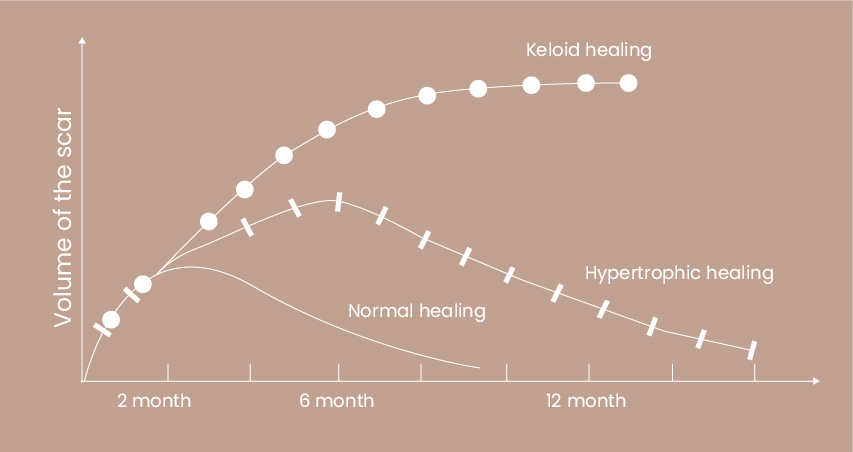
At first, this highly inflammatory scar is accompanied by redness and itching. Its volume develops rapidly for three to six months, but remains confined to the limits of the original incision, unlike keloid scars (see below).
How does it evolve ?
After a stagnant phase, the volume of the scar will begin to decrease, and the maturation process may take up to 2 years (18 to 24 months in general). These scars are essentially an aesthetic problem. In case of previous pathological scars, an adapted prevention strategy is recommended (pressure therapy, injection of corticosteroids in the scar, compressive dressings, silicones, lasers etc.)

Keloids scars
How does it look like ?
They are voluminous, sometimes painful and can itch. The specificity of these scars is that they extend well beyond the initial incision area.
Zones and risk factors ?
Their localization are common in the face, the neck, the ears, the shoulders, the thorax, and the anatomical areas where the skin is thick.
Patients with a dark skin phototype are particularly at risk. A genetic anomaly could also be at the origin of these complications.
When does it come to light ?
They appear later than hypertrophic scars up to one year after the onset of the initial lesion and they do not regress spontaneously. They often are resistant to treatments, even to surgical removals and may reappear again after.
What to do ?
In case of keloid history, a strategy of prevention is recommended (pressure therapy, injection of corticosteroids in the scar, compressive dressings, silicones, lasers etc.).
It may even question the risk and benefits of an aesthetic surgery.

Adherent and/or retractile scars
How does it look like ?
It is like fibrous cords that are relatively stiff and slightly elevated relative to the level of the surrounding skin.
These are scars that are “curled up“ like.
Where are they located ?
They will be found in areas of high mobility, joints, and bending folds.

Each scar is unique and depends on both its location and numerous individual factors.
Phototypes at risk
Patients with a high phototype, such as Hispanics, Asians, Indians, or Africans, are scars localized for scarring abnormalities.
Cutaneous healing in these patients is characterized by a intensive and longer inflammatory reaction, the body “over-reacts” to heal the wound.
Scars on the face
Scars localized on areas of muscular tension and exposed to sunlight, such as the face or neck are more likely to evolve unfavorably.
Because these scars are also clearly visible and exposed, their appearance may present a particular concern.
Scars localized on the chin, cheek, forehead and nasal tip are more prone to become hypertrophic and enlarged compared to those located on other areas of the face.
Likewise, areas near the moving regions of the face have an increased risk of generating enlarged scars due to continuous traction on the surgical incision.
Please note: To limit the tensile forces exerted on the scar, your surgeon will always make the surgical incision taking into account areas of tension.

